A GUIDE TO ROBOT-ASSISTED LAPAROSCOPIC RADICAL PROSTATECTOMY (RALRP)
RALRP is surgery performed to treat localised prostate cancer. It is performed under general anaesthetic and takes about 3 hours. Six small cuts are made in the abdomen, and a camera scope, as well as laparoscopic instruments, are placed through these port sites. These instruments are then attached to robotic arms on a device called a daVinci robot, and the surgeon then controls these robotic arms from a separate console. This way of removing the prostate gland is becoming more and more popular because the robotic arms provide a greater degree of steadiness and dexterity for the surgeon, as well as an enhanced and magnified view of the prostate gland and surrounding structures. This can allow a more precise operation. However, it is important to emphasise that this is still major surgery with potential risks and side-effects and that it is still the surgeon, Dr Patel, who performs your operation.
The overall cure rate for men undergoing this operation is high, around 85-95%.
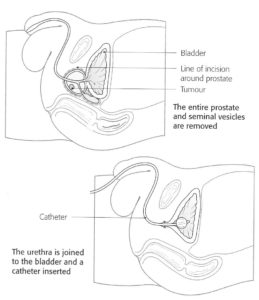
The entire prostate gland and seminal vesicles are removed in the operation. Sometimes, regional lymph nodes are also removed as part of the surgery. The bladder is then reattached (anastomosed) to the urethra so that urine is still passed through the penis postoperatively. However, semen is no longer produced and you will be sterile.
Most patients can go home after 1-3 days, but a urethral catheter (see diagram over) is left in place for about 7 days after the operation to allow the anastomosis to heal up properly.
Partial or complete loss of erections (impotence) can be a side-effect of surgery but many patients are suitable for “nerve-sparing surgery” whereby the nerves that control erections are protected, and this can often allow recovery of erections after surgery. The success of nerve-sparing surgery depends primarily on the patient’s age at operation, but also on their sexual function prior to surgery, anatomical variations, and early commencement of medical treatment after surgery. It can take up to 18-24 months for maximum recovery of erections after surgery.
Incontinence (involuntary urine leakage) can occur after surgery also, but the vast majority of men will gain good urine control within the first 6 months after surgery, especially if they perform male pelvic floor exercises daily after the catheter is removed. Dr Patel’s office will provide you with a brochure on pelvic floor exercises. The risk of permanent and significant leakage beyond 12 months after surgery is only around 2-3%, and if it does occur, it can often be permanently improved by a small operation called “transobturator sling placement”.
DVT and pulmonary embolism (blood clots in the legs or lungs) can occur after any surgery and are potentially life-threatening. The risk is low (less than 2%) and appropriate precautions will be taken to minimize your risk.
Blood transfusion is required in less than 5% of operations performed by Dr Patel
Rarely, the rectum, or back passage can be damaged during surgery (less than 1%). This may require further surgery to repair any injury.
Sometimes fluid collections in the pelvis (lymphocoele or haematoma) can occur after radical prostatectomy and may need to be drained out as a separate procedure (less than 5% chance)
After surgery, the prostate is examined by a pathologist to see if all the cancer is contained in the specimen. If so, then no further treatment should be required.
PSA (Prostate Specific Antigen) should be undetectable in your blood by about 6-8 weeks after the operation, if the cancer has been fully cleared. Dr Patel will advise you when to have your PSA blood test checked after the operation, and provide you with a pathology request form. You will need to have a PSA blood test periodically, for about 8 years after surgery.
You will need to avoid any very strenuous activity or heavy lifting for 6 weeks after your operation.
THIS INFORMATION COVERS THE MAIN ISSUES RELATED TO ROBOT-ASSISTED RADICAL PROSTATECTOMY AND SHOULD BE SEEN AS AN AID TO YOUR DISCUSSIONS WITH DR PATEL REGARDING YOUR TREATMENT.
Download a printer friendly version of this page